Health
Care Technology Meets Mobile Applications
Mobile Application to Prepare
for Future Stroke Scenarios
Bradley James Shedd
Southern Polytechnic State
University
Major: Information Technology
Date: November 6, 2012
Abstract
On
July 31, 2012 I witnessed a loved relative have a severe stroke and heart
attack. I want to research and
report if there are any types of applications on mobile devices that help stroke
victims or perhaps prevent future strokes.
The worst part about being in a hospital is waiting for the doctor to
give a final diagnosis and discharge the patient.
The scope of this report is to discuss how the doctors use their mobile
technology. The health field has
this technology available to doctors, but I want to find an application to help
patients at their home. The
application would allow the stroke victims to announce what they want without
speaking, by touching pictures of daily activities on some device like a
Personal Digital Assistant (PDA) or a smart phone.
We live in a world that is filled with cutting edge technology at an
affordable price for everyone.
Every friend of mine, including myself, has a smart phone and home computer.
The health field has found a way to keep
in touch with your doctor through a webcam on your computer or a camera on your
cell phone. The Health Insurance
Portability and Accountability Act of 1996 (HIPPA) has guidelines to follow to
keep confidential health files sent over wireless networks secure.
I would like to find out what current health field technology there is
today, and see if there are some inventions in mobile applications that will
improve the stroke patient’s recovery process.
1
Introduction
 The
fourth most leading cause of death in the United States of America is
cerebrovascular diseases, also known as strokes.
The first leading cause was diseases of the heart (Hoyert, 2012).
Since cellular devices are becoming very popular in the United States, it
is important for Americans to know how they can use their cell phone to help
improve their health. The PDA is
being used by doctors to monitor patients while making their rounds at the
hospital. There is a portable
device that can store, view, and record the new progress of each patient for
review by the doctor.
The
fourth most leading cause of death in the United States of America is
cerebrovascular diseases, also known as strokes.
The first leading cause was diseases of the heart (Hoyert, 2012).
Since cellular devices are becoming very popular in the United States, it
is important for Americans to know how they can use their cell phone to help
improve their health. The PDA is
being used by doctors to monitor patients while making their rounds at the
hospital. There is a portable
device that can store, view, and record the new progress of each patient for
review by the doctor.
“Although primary stroke centers (PSCs)
are equipped with the resources and personnel to provide patients with acute
stroke with a timely, adequate assessment and emergency stroke treatments, they
represent only a minority of all hospitals” (Demaerschalk, 2009).
Every second counts when someone suffers an attack from a stroke.
The patient is confused and may or may not know that a stroke has
happened. When an emergency team of
doctors and nurses are in the room at once, one could be confused as exactly
what has happened. The solution to
this is having a telestroke team that consists of clinical, administrative, and
research members (Demaerschalk, 2009).
“Neurologists, emergency physicians, nurses, and radiologists should
collaborate on the provision of remote care for patients with acute stroke. In
general, telestroke practitioners are board-certified vascular neurologists;
however, no formal requirements for the practice of telestroke currently exist”
(Demaerschalk, 2009). If one
physical therapist is in the room with the patient, the patient could feel more
relaxed.
The act of surviving a stroke
is like fighting from the grasps of hell and the more the patient is oblivious
to this the better. When the
patient is undergoing rehabilitation, the doctor can record and view the
patient’s recovery with a webcam.
“Fisher proposed a hub-and-spoke model of telemedicine-delivered stroke care
designed to enhance the administration of acute stroke therapies” (Demaerschalk,
2009). Now, a doctor can view
several patients at a time and in theory speed up recovery from the stroke.
The doctor may also use their PDA to view the patient practicing physical
therapy from their home.
2
PDA Pros and Cons
Now, when a patient is out of the emergency department and is starting
the recovery process from the stroke, their progress needs to be monitored for
at least three to six months during the brains neurological recovery process.
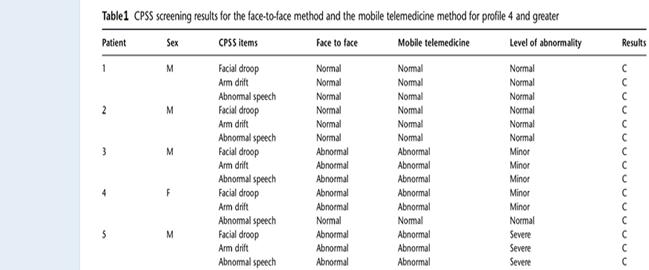
The mobile telemedicine system was introduced in 2009 and streams video
of the patient in rehabilitation to the doctors smart phone.
The doctor is using a Windows 2003 phone with a stylist pen to view the
patient on the phones screen. The
video feed would transmit to the doctor’s phone but with a low bit rate.
This means that the patient could have a facial droop, a side effect of a
stroke, and the doctor would not recognize the facial features on their phone
(Kim, 2009). However, the audio
quality was fine and the doctor could listen to the speech abnormalities (Figure
2).
2.1 HIPPA Protected
The first intention of
instantiating the Health Insurance Portability and Accountability Act of 1996
was to improve portability and continuity of health coverage (Gartee, 2011; pg.
47). The cellular telephone, a
portable phone, is a picture perfect solution to improve portability health
coverage. Two of the four areas of
the Administrative Simplification Subsection of HIPAA, privacy and security, are
questionably at risk when confidential records are being transferred over
cellular airspace (Gartee, 2011; pg. 47).
Since the patients confidential health records are being sent from the
hospitals database streaming live video through the internet, to an access point
or base station and then to the mobile phones VPN there needs to be some
security (Figure 2).
When patient’s records are
the issue the loss of data is a high risk.
Unauthorized access to patient data through a wireless local area network
by an adversary could happen. The
intrusion detection system could fail to detect penetration of an adversary.
The hardware equipment may be improperly set up or installed.
Therefore, HIPPA has
constructed a set of rules for all wireless networks that are located a
hospitals and/or involve the transfer of medical records.
Section 9 of ISO IEC 27002 was recommended in 2005 for all hospitals to
follow with user authentication for external connections (ISO
IEC 27002, 2005). The HIPPA
security implications of Section 9 and 12 include but not limited to: Use
security areas to protect your facilities; control use of assets off-site;
validate data input into your applications; use validation checks to control
processing; prevent information leakage opportunities (ISO
IEC 27002, 2005).
The telestroke video
conference and mobile telemedicine system followed the ISO IEC 27002 protocol.
The mobile telemedicine system uses secure communication over a wireless
network by using a mobile virtual private network (Kim, 2009).
The patient’s information is secured from being leaked to adversaries by
the “mobile VPN protecting IP packets through an IP security protocol and
tunneling over a private network” (Kim, 2009).
3 Health Mobile Technology is Successful
My research has unveiled
exactly what I was looking for that can help stroke victims.
Now a doctor can view live streaming video on their phone of their
patient. This reduces the trouble
of having to travel to the doctor’s office which could be a problem for a stroke
victim if they are home alone. It
would be comfortable to know that a physical therapist can record the patient’s
progress while training in the convenience of the patient’s home.
However, the way this technology is introduced is that the patient is in
the hospital undergoing physical therapy and the doctor is receiving live video
to his/her cell phone. This makes
dealing with more than one patient more convenient for the doctor.
Either way, the quicker the stroke survivor receives medical attention
the better. Now, the doctor can
review the diagnosis of the patient faster than driving to the hospital.
“The system was tested using a PDA-type
phone and smart phone, as shown in Figure 2. Both receiving units were able to
present satisfactory video for the observation of facial droop and arm movement,
and provide satisfactory audio for the detection of abnormal speech” (Mobile App
for Acute Stroke). This device is
not available on the market, but is used in a few hospitals.
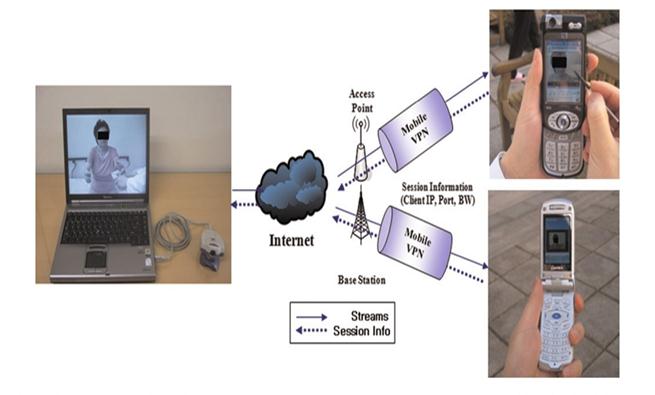
There were five patients all of whom are stroke victims and the table
below shows the results of their progress in the video therapy shown in Table 1.
4 The Future of Implantations
I believe that the new mobile
application can help save lives.
The future is looking forward to microchips that can be implanted into the human
brain to send electric signals that will link the neurons together to command
body movement and improve speech patterns and other side effects of strokes.
The ZigBee is a microchip that is already in the testing phase using
laboratory rats. “The ZigBee link
enables bi-directional communication between the neural stimulator and
controlling equipment on outside. ZigBee is a standard small, low power
radio-frequency communication protocol based on the IEEE 802.15.4 standard,
designed for use in wireless personal area networking (WPAN) applications” (Kim
& Yang, 2010). The microchip is
sending data over a network for the doctors to view how the low electric signal
is helping the brain recover from the stroke.
The ZigBee is looking to be used in human brains to help improve the
three to six month recovery time of a stroke (Kim & Yang, 2010).
5 Conclusion
In conclusion, I recommend on
relying on mobile technology to keep good health by avoiding strokes and heart
attacks. I believe the reason why mobile
applications are needed for stroke victims is because the quicker the victim
gets help and rehabilitation, the faster the recovery process.
“Each second that passes after a stroke the human brain loses 30,000
neurons. If a stroke is left
unattended to for up to 5 hours then the damage to the body are irreversible”
said Mr. Hall our class guest speaker.
We need to take better care of ourselves and monitor our health more than
just relying on doctor visits.
6 Acknowledgements
This research was conducted
for the Foundations of Health Information Technology class at Southern
Polytechnic State University. The
author thanks Dr. Chi Zhang for her knowledge of health information systems and
leadership as a lecturer for Southern Polytechnic State University.
This project was also conducted for the author’s father.
Appendix
Figure 1 -
Example of video chat with stroke patient.
Demaerschalk, B. M. (2009, January). Stroke
telemedicine [Photograph]. Mayo
Clinic Proceedings. Figure 2 -
The system architecture of the mobile telemedicine system for acute strokes.
Kim, D. (2009). A
mobile telemedicine system for remote consultation in cases of acute stroke. [Photograph].
Journal of Telemedicine and Telecare, London.
Table 1 –
Score of the visual feed of the doctors PDA
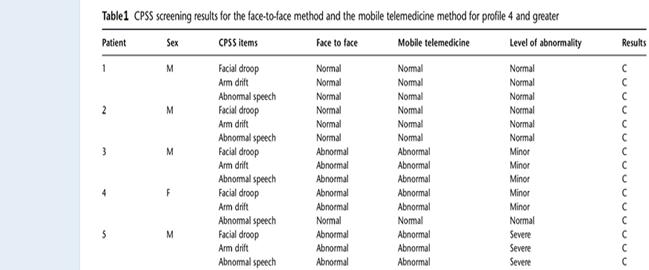
Kim, D. (2009). A
mobile telemedicine system for remote consultation in cases of acute stroke. [Photograph].
Journal of Telemedicine and Telecare, London.
References
Audebert, H. J., Boy, S.,
Jankovits, R., Pilz, P., Klucken, J., Fehm, N. P., & Schenkel, J. (2008,
December). Is mobile teleconsulting equivalent to hospital-based telestroke
services? National Center for
Biotechnology Information. Retrieved October 07, 2012, from
http://www.ncbi.nlm.nih.gov/pubmed/18787198
Boulos, M. N., Wheeler, S.,
Tavares, C., & Jones, R. (2011, April 05). How smartphones are changing the face
of mobile and participatory healthcare: An overview, with example from eCAALYX. National
Center for Biotechnology Information. Retrieved 2012, from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3080339/
Bray, J. E., O'Connell, B.,
Gilligan, A., Livingston, P. M., & Bladin, C. (2010). Is FAST stroke smart? Do
the content and language used in awareness campaigns describe the experience of
stroke symptoms? J. E. Bray et al. Research. International Journal Of
Stroke, 5(6), 440-446. doi:10.1111/j.1747-4949.2010.00484.x
Demaerschalk, B. M., MD, Miley, M.
L., BSc, Kiernan, T. J., MSN, Bobrow, B. J., MD, Corday, D. A., BS, Wellik, K.
E., MLS, ... Richemont, P. C., MD. (2009, January). Stroke telemedicine. PMC.
Retrieved October 30, 2012, from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2664571/
Hoyert, D. L., Ph.D, & Xu, J.,
M.D. (2012, October 10). Deaths preliminary data for 2011. CDC.
Retrieved November 01, 2012 from
http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_06.pdf
Hui-fang ChenChing-yi WuKeh-chung
LinHsieh-ching ChenChen, C. (2012). Rasch Validation of the Streamlined Wolf
Motor Function Test in People With Chronic Stroke and Subacute Stroke.Physical
Therapy, 92(8), 1017. doi:10.2522/ptj.20110175
ISO IEC 27002 2005. (2005,
December 22). ISO 27002 (17799)
Information Security Standard in Plain English. Retrieved 2012, from
http://www.praxiom.com/iso-17799-2005.htm
Kim, D.,
Yoo, S., Park, I., Choa, M., Bae, K., Kim, Y., & Heo, J. (2009).
A mobile telemedicine system for remote
consultation in cases of acute stroke. Journal of Telemedicine and
Telecare, 15(2), 102-107.
Kim, G., Yun, H., Ryu, M., Shin,
Y., Kim, H., & Yang, Y. (2010, December 31). ZigBee-based Wireless
Neuro-Stimulator for Improving Stroke Recovery.National Center for
Biotechnology Information. Retrieved November 01, 2012, from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3214784/
Kume, S., Hama, S., Yamane, K.,
Wada, S., Nishida, T., & Kurisu, K. (2010). Vulnerable carotid arterial plaque
causing repeated ischemic stroke can be detected with B-mode ultrasonography as
a mobile component: Jellyfish sign. Neurosurgical Review, 33(4), 419-430.
Smartphone app enables accurate stroke diagnosis. (2011). Informationweek -
Online, Retrieved from
http://search.proquest.com/docview/867006464?accountid=13751
Srinivas, K., Rani, B., & Govrdha, A. A. (2010). Applications of Data Mining
Techniques in Healthcare and Prediction of Heart Attacks. International
Journal On Computer Science & Engineering, 1(2), 250-255.
Waxer, C. (2010). Mobile App Saves
Lives. Cio, 24(3), 13-14.
 The
fourth most leading cause of death in the United States of America is
cerebrovascular diseases, also known as strokes.
The first leading cause was diseases of the heart (Hoyert, 2012).
Since cellular devices are becoming very popular in the United States, it
is important for Americans to know how they can use their cell phone to help
improve their health. The PDA is
being used by doctors to monitor patients while making their rounds at the
hospital. There is a portable
device that can store, view, and record the new progress of each patient for
review by the doctor.
The
fourth most leading cause of death in the United States of America is
cerebrovascular diseases, also known as strokes.
The first leading cause was diseases of the heart (Hoyert, 2012).
Since cellular devices are becoming very popular in the United States, it
is important for Americans to know how they can use their cell phone to help
improve their health. The PDA is
being used by doctors to monitor patients while making their rounds at the
hospital. There is a portable
device that can store, view, and record the new progress of each patient for
review by the doctor.